Human beings have benefited from vaccinations for over two centuries. The introduction of medicine as a pathway to prevent diseases came in 1796 when Edward Jenner, a country doctor from England, discovered that milkmaids who had been infected with cowpox (the first vaccine) did not show symptoms of smallpox. Fast forward to the late 1800’s through the 1960’s; antitoxins and vaccines were developed to combat major diseases like polio, measles, mumps, tetanus, and more. Throughout the mid to late 1900’s, widespread usage of vaccines proved to be so effective that some diseases were eventually declared eradicated from the U.S, including measles (2000) and rubella (2014). Mumps and whooping cough were never officially eliminated from the U.S. but were nearly forgotten as vaccination rates soared and cases became few and far between. Centuries after Jenner first discovered the smallpox vaccine, inoculations were hailed as critical achievements in public health. It is in this vein that it is alarming (and disturbing) that these diseases have reappeared throughout the globe. A major reason for their come back? Anti-vaxxers.
Anti-Vaxxers and Their Impact in the U.S. and Abroad
The anti-vaccination movement gained traction in 1998, when Andrew Wakefield published a now widely-debunked paper in The Lancet suggesting a link between the MMR vaccine, inflammatory bowel syndrome, and autism. Spoiler alert: there is no link between the MMR vaccine and autism. Yet, the fraudulent linkage remains a selling point for the anti-vaxxer community and continues to have a widespread impact on public health. Outspoken celebrities (with no medical credentials) such as Jenny McCarthy, Jim Carrey, Robert F. Kennedy Jr., and Robert de Niro, continue to incite fear around these disproved and false side effects of vaccination.
State governments are responsible for implementing vaccination requirements for school-aged children and healthcare workers. Parents of school-aged children are able to circumvent these requirements by taking advantage of different state-specific exemptions available to them. California, Mississippi and West Virgina are the only states that accept only medical vaccinations exemptions. The remaining 47 states and the District of Columbia accept nonmedical vaccine exemptions, including for philosophical and religious purposes. Eighteen states offer philosophical exemptions, making it easy for anti-vaxxers to opt out of vaccinations for virtually any reason.
The United States isn’t the only country suffering from a resurgence of vaccine-preventable diseases. The European Centre for Disease Prevention and Control reported on 6, April 2017 that Belgium, France, Germany, Italy, Poland, and Romania are still considered to have endemic transmission of measles. Unlike the U.S., measles was never completely eliminated from Europe. The World Health Organization Regional Office for Europe reported that ongoing measles outbreaks across the region have caused 35 deaths over the past year, including 31 deaths in Romania alone. Along with Romania, Italy is one of the hardest hit countries, reporting 3, 300 cases since June 2016. Low vaccination coverage among these populations is one of the predominant causes of the outbreaks.
Herd Immunity: What Doesn’t Kill You Makes Us All Stronger
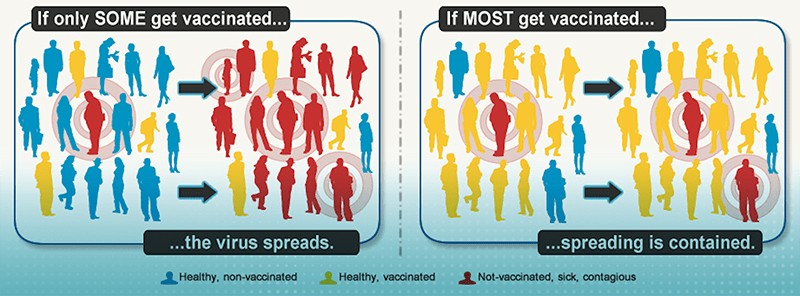
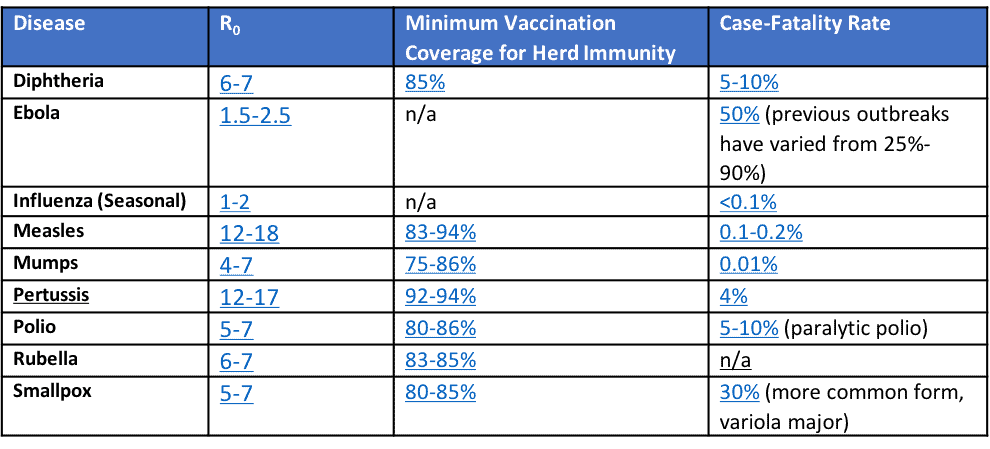
Herd immunity is the protection against an infectious disease, either through vaccination or prior illness, that results from large populations becoming immune to said disease. Not only do vaccinated people protect themselves, they also become part of a human shield to indirectly protect vulnerable populations. In theory, each person in a population does not need to be immune to maintain herd immunity. As noted in the chart below, a minimum threshold of the population needs to be immune to keep the disease in check. As more people buy into the anti-vaxxer campaign and rely on the herd to protect themselves (and their children), vaccination coverage in certain communities can drop below the minimum required to achieve herd immunity, putting the community at risk of an outbreak of these preventable diseases.
Basic Reproduction Number: Predicting Disease Outbreaks
The basic reproduction number, R0, describes the average number of secondary cases an infectious disease causes over its infectious period in a totally susceptible population. For example, measles has an R0 value of 12-18, meaning that one case of measles will generate 12-18 more cases. The effective reproductive number, R, can be estimated for a specific population, given their susceptibility. For populations that are 100% vaccinated, R will drop to essentially zero. Diseases with an R greater than one will persist in a population and potentially cause an outbreak or epidemic. Notably, we can’t compare two different diseases based on their R, as the numbers are often calculated after a specific epidemic and are dependent on the parameters of that specific event. Regardless, the basic R0 gives an idea of whether a disease will take hold in a population, especially if the minimum threshold of vaccination coverage is not met. The real danger of the anti-vaccination movement comes when vaccination rates for the following preventable diseases drop below the minimum vaccination coverage for herd immunity. The lower the vaccination coverage goes, the more secondary infections occur, and the worse an outbreak becomes.
Contrary to what we may think, the vast majority of school-aged children DO get vaccinated each year. According to the CDC, the median Diptheria-Tetanus-Pertussis (DTaP) vaccine coverage was 95% and 47 states reported at least 90% Measles, Mumps, and Rubella (MMR) vaccine coverage among kindergartners during the 2015-2016 school year. Although many people think of primary schools when they hear about vaccinations, college campuses are at risk too, as they provide places where many people across the world and country live in close contact with each other. Recently, the University of Texas, which only requires international students to receive the mumps vaccine, reported 11 cases of mumps on campus since June 19th, 2017.
This leads us to an important question: if an overwhelming majority of children are vaccinated, why are we seeing outbreaks of vaccine preventable diseases? The majority of United States outbreaks can be attributed to two causes:
- Diseases are brought into the United States by travelers (including Americans) that contracted the infection abroad. For example, the Disneyland measles outbreak that began in late 2014 resulted in 147 cases. The outbreak is attributed to an overseas traveler catching the infection abroad and transporting it back to the U.S.
- Low immunization coverage tends to occur in pockets, putting entire populations at risk when coverage dips below the minimum threshold necessary to keep a disease in check.
Case Study: 2017 Minnesota Measles Outbreak
The 2017 Minnesota measles outbreak is a quintessential example of what can happen to populations with low vaccination coverage. (The existing immunizations statute in Minnesota does not outwardly recognize religion as a reason for claiming an exemption, however, the non-medical exemption may include religious beliefs.) The outbreak was largely confined to a group of Somali immigrants, whose vaccination rates declined to approximately 40% in 2017, amid fears of a vaccine-autism linkage. As seen in the above table, a community needs to have a minimum of 83-94% vaccination coverage to maintain herd immunity against measles. This community had less than half of the coverage necessary to protect them from infection. Among 79 total cases in this measles outbreak, 71 were confirmed to be unvaccinated. Measles is highly infectious, so it’s no surprise that the disease took hold in a community of unvaccinated people.
Luckily, the outbreak remained relatively confined within this community. Why? It’s difficult for an infectious disease to take hold in a population where the vast majority of people are immune (see above diagram).
Vaccination: A Societal Responsibility
At the end of the day, people have the right to refuse vaccinations (assuming they have a valid exemption). However, the science is present and verified: barring a medical condition, you need to be vaccinated to protect both yourselves and the vulnerable populations who can’t be vaccinated. If vaccination coverage continues to fall in the United States, we’ll be seeing more outbreaks of diseases that require a lower threshold to keep the disease in check, such as mumps and rubella. As Dr. Zsuzsanna Jakab, WHO Regional Director for Europe, stated, “Everyone has a role to play: the system works when the entire society is committed to immunization.”
