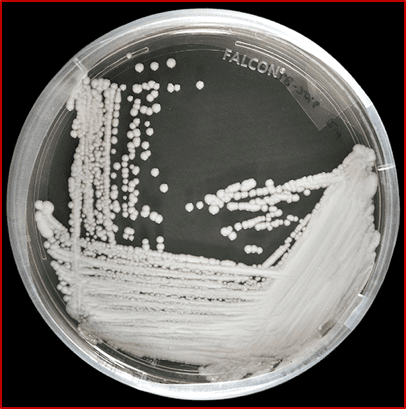
Hospital-acquired infections are a common cause of patient illness and death around the world, including in well-developed hospital systems. The United Kingdom recently reported on an outbreak in which over 200 patients were colonized with the fungus Candida auris (C. auris). Colonization occurs when the fungus is detected on a patient’s skin, and patients may later develop a life-threatening infection. In the UK outbreak, approximately 25% of colonized patients developed an infection, including 27 who developed bloodstream infections. Globally, it is unclear what percentage of colonized patients develop an infection – but for those who do, the fatality rate may be as high as 60%. Complicating the outbreak, many people who have been colonized do not show symptoms and are more difficult to identify and quarantine. Patients experiencing long-term hospitalization, those with lines or tubes entering their body, or who have previously received antimicrobial medications are at higher risk of infection.
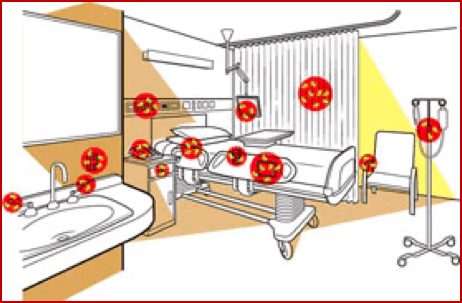
According to Dr. Tom Chiller, chief of the Mycotic Diseases Branch at the CDC, C. auris is primarily transmitted within hospital settings. Outbreaks are caused by contact with contaminated surfaces and affected patients. The fungus is very resilient and can easily gain a foothold on equipment and surfaces within the hospital or nursing home. Some strains of C. auris have proved resistant to first, second, and third-line antifungals and the CDC warns that patients may remain colonized for months, or even indefinitely.
C. auris was only discovered in 2009 and has become increasingly common since then, spreading to more than 12 countries including the US. Earlier this year, the Center for Disease Control’s (CDC) acting Director Dr. Anne Schuchat cautioned that case counts were on the rise in the United States as well. The latest statements from the CDC report 98 infections identified in the United States as of July 2017 – up from 61 cases in April 2017 when the CDC issued its warning.
These infections are not limited to substandard medical facilities; hospitals across the US and UK have been impacted. The risk of infection for travelers is low, but patients in the US and abroad should be aware of C. auris among other hospital-acquired infections and seek medical care at hospitals with strict infection control protocols. An underdeveloped understanding of Candida auris means that control measures are still being developed.
For now, the CDC is recommending that colonized patients be placed in a single-patient room and be cared for using standard contact precautions. Additional work is necessary to improve detection and infection control practices at healthcare institutions around the world.
