On January 10, 2020, VIGILINT first reported a new strain of a coronavirus connected to a cluster of pneumonia cases linked to Wuhan, China.
No one could have predicted the year that would follow. As of publishing, worldwide cases have reached 104 million with 2.27 million deaths.
VIGILINT looks back at the critical events that shaped the COVID-19 pandemic of 2020 in a two-part series COVID-19 One Year Later. This article focuses on the two best and two worst handlings of the COVID-19 crisis and what we can learn from them.
Rapid Spread – Early Timeline
In the following weeks and months after the initial virus discovery on December 31, 2019, VIGILINT followed the disease progression, which eventually landed in Washington State by January 21. The first 5 cases in the US were travelers returning from Wuhan, China, or near the Hubai Province. As travel advisory warnings to China rolled out, cases rapidly increased far from Wuhan’s point of origin for the first time. The northern region of Italy suffered a severe bout of community spread, as did South Korea.

Dr. Nancy Meissonier, the Director of the CDC’s National Center for Immunization and Respiratory Diseases, announced on February 26, “it is not so much a question of if this will happen anymore, but rather more a question of exactly when this will happen. And how many people in this country will have a severe illness.”
On March 11, in response to the alarming spread and severity of the disease worldwide, the WHO declared COVID-19 a Pandemic. The Director-General, Tedros Adhanom Ghebreyesus, expressed concern over the “alarming levels of inaction.” In the US, early severe missteps and delayed action shifted America’s national pandemic approach from a scientific emergency plan to a passive, detached political strategy embodied by the central organizing principle of “reacting when the full impacts are visible.”
A year into this, and January 2021 has been the deadliest month in the US, with nearly 95,000 lives lost. Hospitals are suffering, and citizens are growing weary of continued restrictions. Did it have to get this bad? Almost every country suffered mass causalities, but some countries handled the response much better than others.
Nation’s Handling of the COVID-19 Crisis
As COVID-19 cases began to grow exponentially, governments’ responses varied from lax, to severe, to delayed, to downright chaotic. The two countries who were considered best prepared for such an event were the US and the UK. And yet, they are among the countries with the highest death rates. Mitigation strategies proved to depend more than just the nation’s wealth, scientific achievements, or robust public health infrastructure. Strong leadership, cohesive communication, swift action, and citizen solidarity are among the defining factors in countries with fewer case and death counts.
Numerous studies have assessed which countries managed the crisis the best and which countries should have done better. Here is VIGILINT’s list:
The Best
Taiwan: An Early Start and Contract Tracing

Taiwan, an island nation with 23.78 million citizens, managed to keep cases under 800 with only 7 COVID-19 related deaths and doing so without a lockdown. As the rest of the world was learning about the novel coronavirus in mid-January, Taiwan had already ceased air travel from much of China, implemented quarantine measures, and “quadrupled production of face masks in one month.” In the United States, it was not until April 4 that the CDC reversed course and recommended cloth masks in public as a legitimate protective measure. Wearing masks to prevent illness is commonplace in East Asian countries, so citizen compliance was a non-issue.
Taiwan’s proximity to China and the pandemic epicenter allowed for an early containment strategy. Pre-planning mitigation protocols learned mainly from the SARS pandemic in 2003 were executed quickly. Notably, Taiwan’s extensive contract tracing techniques, like mobile Sim-tracking, enabled the government to monitor people in quarantine, to make sure they stayed in quarantine. Major privacy concerns aside (for now), these early methodologies influenced the island’s low case count.
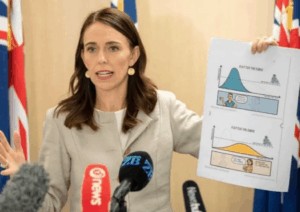
New Zealand: Complete Elimination Plan and National Unity
In a Performance-Based Index from Sydney’s Lowey Institute, New Zealand topped the list out of almost 100 countries for their successful handling of the pandemic. The Lowy Institute remarked: “In general, countries with smaller populations, cohesive societies, and capable institutions have a comparative advantage in dealing with a global crisis such as a pandemic.” The country with the highest number of deaths, the United States, has a population of 330 million, soaring over New Zealand’s 4 million. And other hard-hit European countries have population ten times larger than the island nation.
New Zealand’s geographic isolation in the South Pacific Ocean makes border restrictions easier to control. Tourist season brings an influx of European and Chinese travelers to the island every year, so the country enacted border control policies in early February to delay the eventual spread. Community spread began in mid-March, and modeling showed an influx of cases would choke the healthcare system and disproportionately affect the Maori and Pacific peoples.
Informed by “science-based advocacy,” Prime Minister Jacinda Arden instituted a “level 4” country-wide lockdown on March 26 for seven straight weeks. The goal – complete elimination. Like Taiwan’s previous SARS experience, New Zealand followed a “flattening the curve” pandemic strategy from an influenza outbreak in 2017. New Zealand‘s total case count of 2,229 cases and 25 deaths are among the lowest of developed countries.
Prime Minister Arden’s empathic and honest call for the country to unify as a “team of 5 million” is credited for citizen adherence to the restrictions.
The Worst
The United Kingdom: Fumbled Early Delays and Losing Position
The country suffering the worst death toll in Europe went into lockdown for the third time in nine months on January 5, 2021. The stay at home order extended to Wales, Northern Ireland, and most of Scotland.

A new, more contagious strain was running rampant, and hospitals could not keep up. The number of people hospitalized with COVID-19 was 40% higher in early January than at its peak last spring. With over 3.4 million cases and 107,000 deaths, the current lockdown is what many hope is the final push to get the virus under control.
Although markedly delayed compared to its European counterparts, Britain’s first lockdown of 2020 started to show signs of containing the virus by summer. By then, lessons learned from delayed border closures, inadequate testing programs, and the massive loss of life seemed to take hold. The government knew of the dire winter warnings and the possibility of mutations. Unfortunately, the country did not move fast enough to apply new restrictions in October, and cases started to surge again. As Ian Boyd, a professor and member of SAGE, put it: “The reality is, there has been a major systemic failure.”
In good news – the UK’s vaccine rollout has been hailed as a success, as 11.7 of the population (8 million people) have received their first shot. The lockdown is expected through March 8, and the nation aims to get as many clinically vulnerable and front-line workers vaccinated by February.
The United States: COVID-19 Impact Denial and Several Botched State-Led Plans
Throughout February 2020, President Trump referred to the disease as a “hoax.” The President also unabashedly nixed concerns about hospitals’ imminent resource shortages. At the same time, leading scientists and infectious-experts called for better testing programs and for American’s to stay at home. The polarizing early mixed messaging between science and government hindered any real chance for the nation to unify in a time of crisis.
In April, Trump announced that the states would lead containment efforts and that the Federal Government would play the “backup role.” The US’s pandemic performance was, as a result, a disjointed, “patchwork” of responses by state and local governments “with states, counties and cities all filling the vacuum created by the lack of an overall national response.”
The states’ stay-at-home mandates and testing programs were as varied as to when and how the states reopened. Some states like Texas and Florida let their stay-at-home orders expire despite not meeting recommended guidelines. As cases started to surge again, leaders in those states faced mounting scrutiny to reinforce restrictions. It became commonplace for a state leader to make a U-turn on messaging.
The CDC urged masks, yet the White House downplayed their effectiveness. The Texas governor claimed there is “no reason to be alarmed” while 18 people died in his state every day. The highly-politicized rhetoric of minimizing the virus’s impact to reopen the economy was unique to the US. Other countries, even the UK, delivered key messages of unity to bring the virus under control. The leaders’ inability in the highest office to regard COVID-19 for what is – a deadly, contagious disease – is a disaster.
The Lowy Institute ranked the US at number 94 out of 100. The study did not include China due to a lack of public data on testing in that country.
VIGILINT’s COVID-19 One Year Later, Part II will cover the areas of testing and vaccines.
