For years, public health experts have warned that a rising tide of antibiotic resistance could make once-manageable diseases into untreatable “superbugs.” Now, an illness most would rather ignore is approaching that threshold and demanding global attention: gonorrhea.
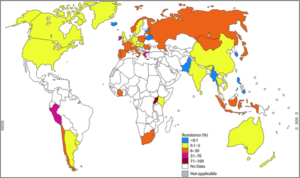
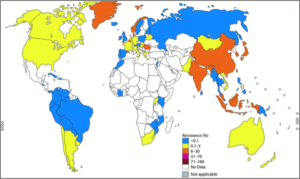
Gonorrhea, a sexually-transmitted bacterial infection, is already a heavy burden on public health agencies. The WHO estimates that at least 78 million people contract the disease each year, and those millions of cases have become harder to cure. Gonorrhea adapts rapidly to treatment options, and now only a combined dose of injected ceftriaxone and oral azithromycin is recommended. Ceftriaxone is the only recommended drug in a category called extended-spectrum cephalosporins (ESCs), which represent the last line of treatment for gonorrhea. Unfortunately, even the current recommended treatment course is in danger. New WHO-sponsored research reveals that in 2014, 51% of observed countries report increased resistance to ESCs like ceftriaxone, and 78% report increased resistance to azithromycin. Ceftriaxone has failed to treat some cases of multi-drug resistant gonorrhea in Japan, France, and Spain, and even the recommended ceftriaxone-azithromycin dual therapy has failed in at least one case. These “superbug” strains will only grow more common as gonorrhea continually adapts to antibiotic treatment. Many countries in Africa and Latin America have not provided data to the WHO, despite being hardest-hit by new gonorrhea infections. Given the limited knowledge of the resistance patterns in these areas and response to drug resistance in those areas, it is very likely that the problem is worse than WHO data suggest.
Widespread untreatable gonorrhea would mean more than embarrassment and discomfort: left untreated, gonorrhea can cause serious health problems for men and women. In women, gonorrheal infections can develop into pelvic inflammatory disease, potentially causing internal abscesses, chronic pain, life-threatening ectopic pregnancies, and infertility. In rare cases, gonorrhea can develop into disseminated gonococcal infection, which can be life-threatening. Infected pregnant mothers can pass gonorrhea to their babies, putting newborns at risk of blindness and a life-threatening blood infection. Untreated gonorrhea also increases the likelihood of contracting and transmitting HIV. Though up to 40% of infected men and over 50% of infected women display no symptoms, untreated asymptomatic cases can still develop dangerous complications and spread undetected.
What can be done to prevent the global spread of drug-resistant gonorrhea? Unfortunately, public health organizations and drug companies have few answers. Antibiotic drug research suffers from chronic underinvestment, and only three medications are currently in development, all in the trial stage and years away from commercial use. Vaccine development is in even earlier stages. Public health organizations like the WHO are in desperate need of additional funding for case identification, effective treatment provision, and research and development for new medications.
While the world waits for additional public health funding, individuals should employ strong precautions to prevent infection. Individuals should either abstain from sex or use latex condoms during vaginal, anal, and oral sex, especially during travel. Individuals who are sexually active should receive STD testing regularly, as many cases are asymptomatic. Anyone experiencing genital sores, genital rash, penile or vaginal discharge, or burning or discomfort while urinating should seek STD testing and treatment immediately, then inform sexual partners of any diagnosed STD.
VIGILINT will continue to update clients about the status of antibiotic resistance in gonorrhea and other infections. Clients should always take aggressive precautions to prevent infection; prevention is always preferred to costly and complex treatment.
