The Centers for Disease Control (CDC) has reported the first US cases of a drug-resistant fungus, which causes skin infections, rashes, and lesions. The first known patients, two women in New York City, have experienced symptoms including lesions on their backs, thighs, buttocks, and genitals. The fungus responsible, Trichophyton indotineae, is highly contagious and poses a significant public health risk. While there is currently no cause for alarm, an awareness of T. indotineae, how it is transmitted, and its symptoms and possible treatments are vital for medical intelligence.
What is Trichophyton indotineae?
T. indotineae is a fungus from a family of fungi that may cause skin infections–or dermatophytosis–in human beings, including athlete’s foot. T. indotineae causes the kind of infection commonly thought of as ringworm, albeit in a much more contagious and virulent way.
Originating in either South or Southeast Asia, likely due to the overuse of antifungal medications, T. indotineae is “epidemic” on the Indian subcontinent. Until recently, however, cases of T.indotineae and its resultant ringworm infection were rare outside of that region. However, the recent infections in NYC include one individual who had no recent history of international travel, indicating that local transmission may be occurring.
Symptoms and Treatment of this drug-resistant fungus
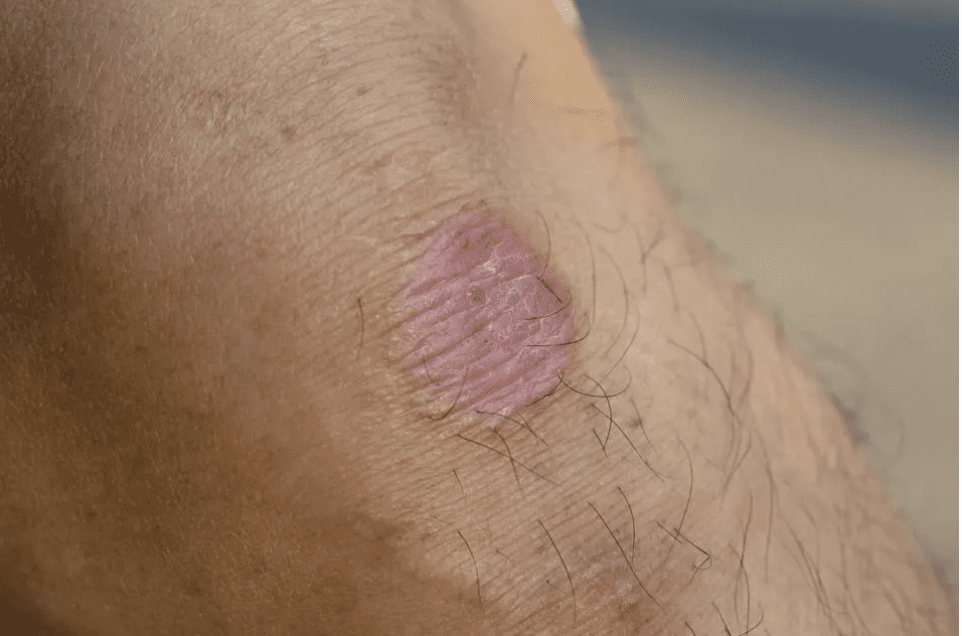
Ringworm is, perhaps unfortunately, familiar to many of us. This familiarity should not breed complacency; T. indotineae presents clinically with a host of symptoms which may become severe, and have been described by Indian dermatologists as “recalcitrant” and drug-resistant. The symptoms of T. indotineae may include the following:
- Itchy skin
- Ring-shaped rash
- Red, scaly, cracked skin
- Hair loss
- Lesions and open sores on infected/impacted areas of the body. These may be intensely itchy, pressure-sensitive, or painful.
The concerns around T. indotineae go beyond those for “regular” ringworm due to this particular fungal infection’s resistance to conventional antifungal treatments. As an illustration, let’s take a look at one of the first US cases. The patient, who first sought medical help in late 2022, was initially treated with a variety of OTC products and topical treatments, including hydrocortisone 2.5% ointment and diphenhydramine, clotrimazole cream, and terbinafine cream. When these failed to produce the desired result, her physician referred her to a dermatologist who prescribed a four-week course of terbinafine, which was likewise ineffective. A subsequent course of griseofulvin proved partially effective, resulting in an 80% reduction in symptoms.
Currently, the only treatment shown to treat T. indotineae ringworm is itraconazole (Onmel, Sporanox) which is currently undergoing consideration by the CDC and other agencies. A current recommendation from the American Academy of Dermatology Association is 100 mg of itraconazole twice daily for 4 to 8 weeks, with the advisory that some patients may require up to 12 weeks of treatment. At this time, recommended second-line agents may include fluconazole and griseofulvin, with luliconazole and voriconazole cream as possible topical treatments.
Precautions and Popular Responses
At the time of this writing, no T. indotineae-specific precautions have been issued by the CDC. However, their generalized ringworm prevention guidelines are likely to be effective in curtailing spread of this drug-resistant fungus, and should be followed by anyone concerned about this disease:
- Keep your skin clean and dry.
- Wear shoes that allow air to circulate freely around your feet.
- Don’t walk barefoot in areas like locker rooms or public showers.
- Clip your fingernails and toenails short and keep them clean.
- Change your socks and underwear at least once a day.
- Don’t share clothing, towels, sheets, or other personal items with someone who has ringworm. This includes athletic and sporting equipment.
- Limit contact with pets and other animals you don’t know, and wash your hands thoroughly after petting or playing with animals including your own pets. If your pet shows signs of ringworm, consult a veterinarian as soon as possible.
To reiterate, there is no cause for panic or excess alarm at this time. Awareness and the reasonable precautions outlined above are adequate to keep us all safe for the time being.

Image: HBO Max
The Last of Us
This is an interesting moment for public health concerns to focus on a fungal infection, as public awareness of the dangers stemming from fungi may be at an all-time high. This is due in part to the lingering public worries about the COVID-19 pandemic but has a great deal to do with the popularity of the HBO series The Last of Us. Starring Pedro Pascal and Bella Ramsey, The Last of Us follows the lives of two characters making their way across a post-apocalyptic American landscape caused by a pandemic Cordyceps fungal infection. In the fictional world of The Last of Us, the Cordyceps infections turns some of the afflicted into violent zombies who attack survivors of the pandemic and resulting societal collapse.
While this outcome is unlikely with this drug-resistant fungus, the positive audience response to The Last of Us and the star power held by Pascal and Ramsey have heightened public awareness of fungal infections. Employers, businesses, and public health providers should therefore arm their audiences with accurate, up-to-date information. At VIGILINT, we offer our clients access to cutting-edge medical intelligence, and we will continue to monitor this particular situation accordingly.
